3D Bioprinting: Printing human organs
Imagine a world where waiting for an organ transplant is a thing of the past. A future where human organs and tissues are not only available but can be customized to meet individual needs. This isn’t science fiction; it’s the reality being shaped by 3D bioprinting technology. By combining cutting-edge printing techniques with biological materials, scientists are pioneering methods that could revolutionize medicine as we know it.
3D bioprinting holds incredible potential for creating functional human organs, offering hope to millions on transplant waiting lists. As researchers delve deeper into this fascinating field, they’re uncovering endless possibilities and raising important questions about ethics and safety. Let’s explore what 3D bioprinting really means, its advantages, current applications in medicine, and the exciting—and challenging—future that lies ahead.
What is 3D Bioprinting?
3D bioprinting is a groundbreaking technology that merges the principles of three-dimensional printing with biological materials. This innovative approach enables researchers to fabricate living tissues and even organs layer by layer.
At its core, 3D bioprinting uses bioinks—substances made from cells and biomaterials—that mimic the natural extracellular matrix found in human tissue. By depositing these bioinks through specialized printers, scientists can create intricate structures resembling real organs.
This process goes beyond mere replication; it aims to produce functional tissues that can integrate seamlessly into the human body. With precision engineering, it’s possible to control cell placement and growth patterns, paving the way for personalized medical solutions.
As this field evolves, it bridges biology with advanced manufacturing techniques, promising profound changes in how we approach healthcare challenges like organ shortages and disease treatment.
Advantages of 3D Bioprinting
3D bioprinting offers remarkable advantages that could revolutionize medicine. It allows for the creation of complex tissues and organs with precise structures, mimicking natural human anatomy.
One significant benefit is the reduction of transplant rejection. By using a patient’s own cells, compatibility improves dramatically. This personalization addresses one of transplantation’s greatest challenges.
Moreover, 3D bioprinting enhances research capabilities. Scientists can create accurate models to study diseases or test new drugs without relying solely on animal testing.
The speed of production is another advantage. Traditional organ harvesting takes time and often involves lengthy waiting lists. With bioprinting, viable options can be available rapidly, potentially saving countless lives.
This technology paves the way for innovations in regenerative medicine. Instead of merely treating symptoms, we might develop solutions that restore function by rebuilding damaged tissues directly within patients’ bodies.

The Process of 3D Bioprinting
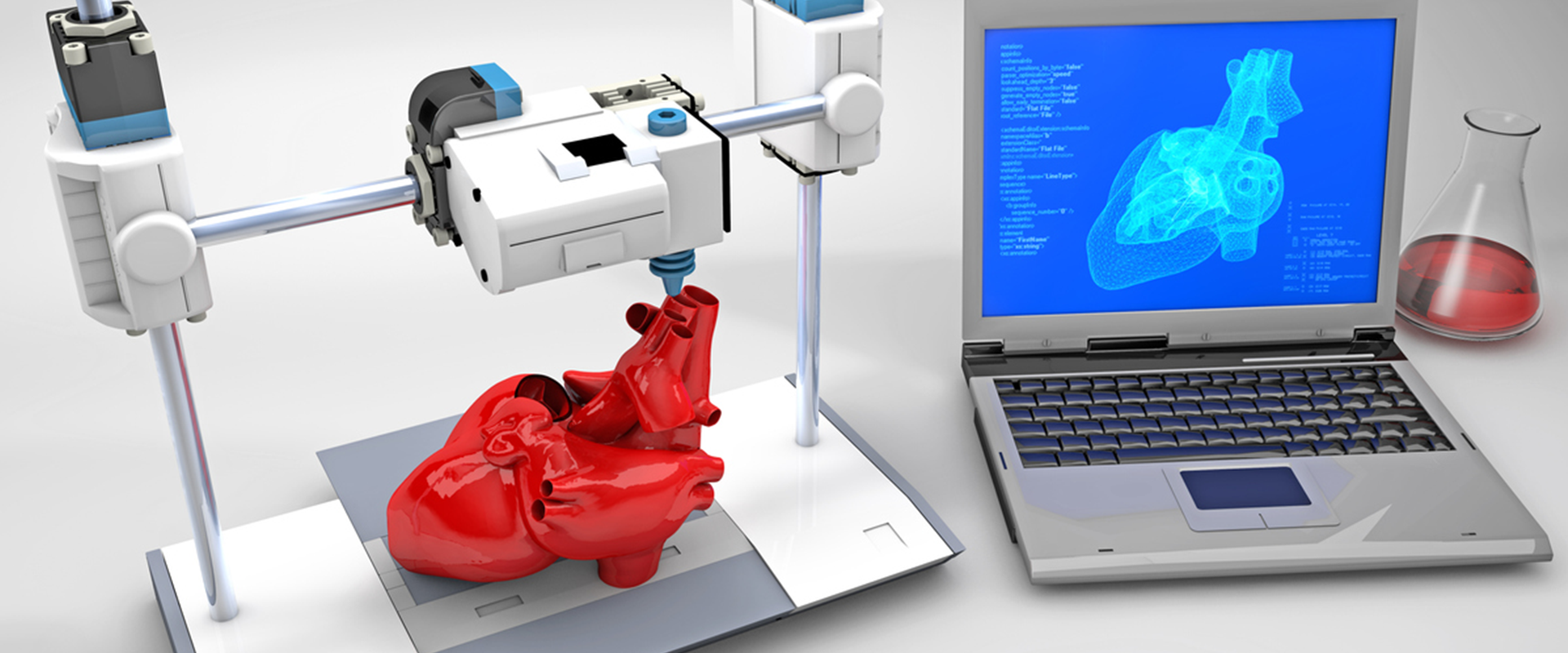
3D bioprinting involves a fascinating blend of technology and biology. The process begins with creating a digital model of the desired tissue or organ. This blueprint serves as the foundation for the printing phase.
Next, bioinks—composed of living cells and biomaterials—are prepared. These bioinks can mimic various biological structures, providing essential support to living cells during development.
Once everything is ready, the printer layers these bioinks meticulously. Each layer builds upon the last, gradually shaping complex tissues that closely resemble natural organs.
After printing, additional steps ensure cell viability and functionality. Culturing in bioreactors helps nurture these newly formed tissues until they are ready for further evaluation or transplantation trials.
This revolutionary approach opens new horizons in regenerative medicine by offering personalized solutions for patients facing organ failure.
Current Applications of 3D Bioprinting in Medicine
3D bioprinting is revolutionizing the landscape of medicine. One of its most exciting applications is in tissue engineering. Researchers are now capable of creating layers of living cells to form tissues that can mimic natural organs.
This technology has made strides in developing skin grafts for burn victims. These printed skin replacements not only speed up recovery but also reduce rejection rates, offering hope for countless patients.
Another promising application lies within drug testing and development. Pharmaceutical companies are leveraging 3D bioprinted tissues to test new drugs before they reach clinical trials. This not only enhances safety but also improves efficacy by better simulating human responses.
Furthermore, organ transplantation faces a monumental challenge: donor shortages. Bioprinting offers an innovative solution by potentially producing viable organs tailored to individual patients, drastically changing the future of transplant medicine. The ability to print complex structures like blood vessels even opens doors previously thought impossible.
Future Implications and Possibilities
The future of 3D bioprinting holds immense potential. Imagine a world where organ shortages become a thing of the past. Tailored organs crafted from a patient’s own cells could revolutionize transplantation.
This technology may also pave the way for personalized medicine. Patients could receive treatments designed specifically for their unique biological makeup, enhancing efficacy and reducing adverse reactions.
Beyond organ printing, advancements in tissue engineering can lead to breakthroughs in regenerative medicine. Damaged tissues might be repaired or replaced with precision-engineered alternatives, promoting faster recovery.
As research progresses, ethical frameworks will need to evolve alongside technological innovations. Ensuring equitable access while addressing moral implications will be crucial as we approach this remarkable frontier.
Collaboration between scientists, ethicists, and policymakers will shape how these advancements are integrated into society. The possibilities seem endless as we stand on the brink of transforming healthcare through innovative 3D bioprinting techniques.
Ethical Concerns Surrounding 3D Bioprinting
3D bioprinting holds immense promise, yet it raises significant ethical questions. As technology advances, we must consider the implications of creating human tissues and organs in a lab.
One major concern revolves around consent. Who has the right to donate cells for bioprinting? The boundaries blur between medical progress and personal autonomy.
Additionally, there’s the issue of accessibility. Will these innovations be available only to those who can afford them? This disparity could widen existing healthcare gaps.
Moreover, what happens if printed organs fail or lead to unforeseen complications? Liability becomes a complex topic when discussing responsibility for such outcomes.
The prospect of “designer” organs brings another layer of controversy. It opens debates about playing God and societal impacts on genetic engineering practices. These concerns highlight that while 3D bioprinting is innovative, it requires careful navigation through moral landscapes as we advance into this new frontier.
Conclusion
3D bioprinting represents a transformative step in the field of medicine, bringing us closer to solutions for organ transplantation challenges. With its ability to create complex tissues and organs using a patient’s own cells, this technology holds immense promise for reducing transplant rejection rates and addressing donor shortages.
The advantages of 3D bioprinting are compelling, from enhancing surgical outcomes to enabling personalized medicine tailored specifically for individual needs. As the process continues to evolve, we can expect more refined techniques that will open doors previously thought impossible.
Current applications demonstrate how far we’ve come—researchers are already printing skin grafts and cartilage with impressive results. The future is even more exciting; as innovation marches forward, we may soon see fully functional organs capable of sustaining life.
However, ethical considerations remain at the forefront of discussions surrounding 3D bioprinting. Questions about consent, accessibility, and potential misuse must be navigated carefully as we advance into this new frontier.
As researchers push boundaries and refine their methods, it’s clear that 3D bioprinting has the potential not just to change lives but also save them. Engaging with these advancements thoughtfully could reshape our understanding of health care in ways we are only beginning to imagine.