Tissue Engineering and Artificial Organs

Introduction to Tissue Engineering and Artificial Organs
Imagine a world where damaged organs can be replaced with bioengineered alternatives, allowing lives to be saved and improved. Welcome to the fascinating realm of tissue engineering and artificial organs! This innovative field merges biology with technology,
paving the way for groundbreaking advancements in healthcare.
As scientists unlock new methods to create functional tissues and organs, they are not only enhancing medical treatments but also redefining what it means to heal. Join us as we explore the history, current developments, and future possibilities that stem from
this incredible intersection of science and medicine. The future of organ replacement is here—let’s dive in!

The History and Development of Tissue Engineering
The journey of tissue engineering began in the 1980s. Researchers sought ways to repair or replace damaged tissues using a blend of biology and engineering principles. This innovative field has evolved dramatically since its inception.
Early milestones included the development of scaffolds—structures that provide support for cells to grow on. These became essential in mimicking natural tissue environments. Scientists experimented with various materials, from polymers to decellularized organs, each contributing uniquely to this evolving discipline.
By the late 1990s, breakthroughs in stem cell research opened new avenues for regenerating tissues. The integration of biocompatible materials allowed scientists to create more sophisticated models for organ regeneration.
Today’s advancements reflect a fusion between technology and medicine, enabling researchers to design bioengineered solutions tailored specifically for patients’ needs. Each step reflects an ongoing commitment to solving complex medical challenges through innovation and collaboration.

Advancements in Technology and its Impact on Tissue Engineering
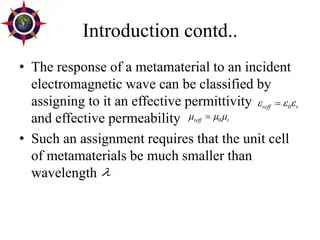
Recent technological advancements have significantly transformed tissue engineering. Innovations in 3D bioprinting allow for the precise layering of cells and biomaterials, creating complex structures that mimic natural tissues.
Artificial intelligence plays a crucial role in this evolution. By analyzing vast data sets, AI helps researchers predict how different cells interact and respond to various environments. This leads to more effective designs for bioengineered organs.
Moreover, stem cell technology has progressed tremendously. It enables scientists to create specialized cell types needed for organ development. This is a game-changer in regenerative medicine.
Additionally, advances in materials science are yielding new biodegradable scaffolds that support cell growth while gradually being absorbed by the body. These innovations enhance the longevity and functionality of artificial organs.
With each breakthrough, we move closer to revolutionizing healthcare through engineered solutions tailored to individual needs.

The Process of Creating Artificial Organs
Creating artificial organs begins with careful planning and design. Scientists identify the specific needs for each organ, whether it’s a heart, kidney, or liver.
The next step involves selecting appropriate materials. Biocompatible substances are essential to ensure that the body accepts these new structures without adverse reactions.
Once materials are chosen, researchers utilize 3D printing technology. This innovative method allows for precise layering of cells and scaffolding, leading to complex shapes mimicking natural organs.
Afterward, tissue engineering techniques come into play. Cells from donors or patients themselves can be cultivated in laboratories to grow onto the scaffold.
Integrating these bioengineered organs into living systems is crucial. Surgeons must carefully transplant them while ensuring proper blood flow and functionality post-surgery. Each phase requires meticulous attention to detail and collaboration across multiple disciplines in science and medicine.

Benefits and Limitations of Tissue Engineering and Artificial Organs
Tissue engineering and artificial organs present remarkable opportunities in modern medicine. They hold the potential to revolutionize treatments for various diseases and injuries, reducing reliance on donor organs. Patients benefit from shorter waiting times and improved quality of life.
However, challenges persist. The complexity of human tissues makes replication difficult. Achieving perfect integration with the body remains a significant hurdle. Moreover, there are concerns regarding biocompatibility; not all engineered tissues function seamlessly within their new environments.
Cost is another factor that cannot be overlooked. Developing bioengineered solutions often requires substantial financial investment, which can limit accessibility for patients who need them most.
Additionally, while advancements continue to emerge, regulatory hurdles slow down progress in clinical applications. Each breakthrough leads to further questions about safety and long-term effects on health—a concern that must be addressed as we push forward in this innovative field.

Current Applications and Future Possibilities
Tissue engineering and artificial organs are already making waves in medical fields. Bioprinting techniques allow scientists to create structures that mimic natural tissues. These innovations offer hope for patients needing transplants.
Current applications include skin grafts for burn victims, cartilage repair for joint injuries, and even vascular grafts that support blood flow. Doctors are using engineered tissues to test drug responses before real-world application, reducing risks associated with clinical trials.
Looking ahead, the potential is staggering. Imagine fully functional hearts or kidneys created from a patient’s own cells—eliminating rejection issues entirely. Researchers are exploring 3D bioprinting at unprecedented levels of complexity.
Stem cell technology continues to evolve, pushing boundaries further into regenerative medicine. The dream of creating bioengineered organs tailored specifically to individual needs may soon become reality, transforming lives while addressing organ shortages globally.

Ethical Considerations
Ethical considerations in tissue engineering and artificial organs are complex and multifaceted. As technology advances, the implications for human life and health become increasingly significant.
One major concern revolves around the source of biological materials used in creating bioengineered organs. Consent from donors is paramount, yet ethical dilemmas arise when considering vulnerable populations or commercial interests.
There’s also the question of accessibility. Will these innovations be available to all, or only a select few? This disparity could deepen existing healthcare inequalities.
Additionally, we must ponder the long-term effects on identity and humanity itself. If we can create artificial replacements that function like natural organs, what does it mean for our understanding of life?
Regulations need to evolve alongside science to ensure responsible practices while fostering innovation. Balancing progress with moral responsibility remains a critical dialogue within this field.

The Cost of Tissue Engineering and Artificial Organs
The cost of tissue engineering and artificial organs is a major consideration. Developing these bioengineered solutions requires significant investment in research and technology.
Materials used can be expensive, especially when biocompatible components are involved. Skilled professionals are needed to design, create, and test these innovations.
Clinical trials further add to the financial burden before any product reaches the market. This lengthy process often stretches over several years, inflating costs even more.
However, once established, artificial organs could save healthcare systems money by reducing long-term treatment expenses for patients with chronic conditions. The initial price tag might seem high, but the potential for better health outcomes is invaluable.
Insurance coverage remains inconsistent across different regions as well. Access to such advanced treatments may not be equitable for all patients based on their socioeconomic status or location.
Investment in this field continues to grow as society recognizes its transformative potential despite high upfront costs.

Challenges and Roadblocks in the Field
Tissue engineering faces numerous challenges that hinder its progress. One significant roadblock is the complexity of human biology. The intricacies of cellular interactions make it difficult to replicate natural tissue structures accurately.
Funding is another hurdle. Research in this field often requires substantial investment, which can be hard to secure. Without financial backing, many promising projects stall before reaching their potential.
Regulatory hurdles also create obstacles. Navigating the complex landscape of approvals and guidelines slows down innovation. Researchers must ensure safety while adhering to strict health regulations, which can delay breakthroughs significantly.
Moreover, ethical dilemmas arise when creating bioengineered organs. Concerns about genetic manipulation or sourcing materials raise questions that society must grapple with.
Public perception plays a crucial role in the acceptance of artificial organs. Misunderstandings and fears regarding bioengineering can limit support for research initiatives and affect funding opportunities.

The History and Development of Tissue Engineering
Tissue engineering has roots that stretch back decades, with early concepts arising in the 1960s. Pioneers like Dr. Joseph Vacanti began exploring ways to create biological structures that could replace damaged tissues.
The field gained momentum in the 1980s when researchers started using biodegradable scaffolds. These materials provided a framework for cells to grow and develop into functional tissue.
In the following years, advancements in cell culture techniques and biomaterials played a crucial role. Scientists learned how to manipulate stem cells, enhancing their potential for regeneration.
By the late 1990s, notable achievements included lab-grown bladders and skin grafts. Each success paved the way for more complex bioengineered solutions.
Today, tissue engineering continues to evolve rapidly, inspired by insights from genetics and nanotechnology. This journey reflects humanity’s aspiration to repair what was once thought irreparable through innovation and creativity.

Understanding Artificial Organs
Artificial organs are remarkable innovations designed to replicate the functions of natural organs. They play a crucial role in modern medicine, offering solutions for patients with organ failure.
These bioengineered devices can be completely artificial or partially combined with living tissue. The latter often involves scaffolds that encourage cell growth and integration into the body.
Common examples include artificial hearts, kidneys, and lungs. Each serves specific functions that mimic their biological counterparts.
The creation process is complex. Engineers must consider biocompatibility, functionality, and durability to ensure these organs perform effectively within the human body.
As technology advances, understanding how these devices interact with human biology becomes vital. This knowledge opens doors for more refined designs that could enhance patient outcomes significantly.
Artificial organs not only address immediate health crises but also pave the way for future innovations in regenerative medicine.

Types of Artificial Organs and Their Functions
Artificial organs come in various forms, each designed to replicate the function of their biological counterparts. One prominent example is the artificial heart. This device can take over pumping blood when a patient’s heart fails, ensuring vital circulation continues.
Another crucial type is the kidney dialysis machine. It performs the essential filtering that healthy kidneys would do, removing toxins and excess fluids from the blood for patients with renal failure.
The growing field also includes innovations like bioengineered skin. Used primarily for burn victims or chronic wounds, it promotes healing by providing a protective barrier while supporting tissue regeneration.
Advancements continue with devices such as cochlear implants. These help restore hearing by converting sound into electrical signals directly sent to auditory nerves.
Each artificial organ serves a unique purpose, enhancing life quality and offering hope where traditional methods may fall short.
Benefits and Limitations of Tissue Engineering and Artificial Organs
Tissue engineering holds immense potential, offering benefits that could transform healthcare. One of the most significant advantages is the ability to create bioengineered organs tailored to individual patients. This customization can improve compatibility and reduce rejection rates.
Additionally, tissue engineering may alleviate the shortage of donor organs. Patients waiting for transplants often face long waits, which could be mitigated by developing artificial alternatives in laboratories.
However, challenges remain. The complexity of replicating natural tissues means that not all engineered solutions function as intended. There are risks associated with manufacturing processes and long-term durability.
Moreover, ethical concerns arise around creating living tissues or organs from stem cells or genetic materials. Balancing innovation with moral considerations poses a dilemma for researchers and society alike.
The cost factor also presents limitations; high expenditures may restrict accessibility for many individuals who need these advanced medical solutions.

Future Possibilities and Advancements in Tissue Engineering
The future of tissue engineering is brimming with potential. As research progresses, scientists are exploring innovative materials and methods for creating bioengineered solutions. 3D bioprinting, for instance, stands out as a revolutionary technique that enables the precise layering of cells to fabricate complex tissue structures.
Another exciting avenue is the integration of artificial intelligence in design processes. AI can optimize scaffold designs, predicting how cells will behave in different environments and enhancing overall functionality.
Moreover, advancements in stem cell technology offer significant promise. These cells can differentiate into various tissues, paving the way for personalized organ creation tailored to an individual’s genetic makeup.
Collaboration between disciplines—biology, engineering, and medicine—will fuel breakthroughs. This synergy may lead to on-demand organ production or even regenerative therapies that restore damaged tissues naturally. The possibilities seem limitless as we venture deeper into this fascinating field.

Ethical Considerations
Ethical considerations in tissue engineering and artificial organs are complex and multifaceted. As scientists push the boundaries of what’s possible, questions arise about the moral implications of creating bioengineered life.
The use of stem cells is particularly controversial. While they hold immense potential for regenerating tissues, sourcing them can lead to ethical dilemmas regarding consent and the status of embryos. This creates a delicate balance between scientific advancement and respecting human rights.
Moreover, issues surrounding access to these technologies must be addressed. Who gets priority when it comes to receiving engineered organs? Socioeconomic disparities could widen if only a privileged few benefit from breakthroughs in this field.
There’s the question of long-term effects on both individuals and society as a whole. Will bioengineered organs integrate seamlessly with human bodies? Or will we face unforeseen complications that challenge our understanding of health? These uncertainties demand thorough discussion among scientists, ethicists, and policymakers alike.

Conclusion
Tissue engineering and artificial organs represent a remarkable frontier in medical science. The journey from initial concepts to groundbreaking advancements showcases human ingenuity and the relentless pursuit of improving lives. As technology advances, we can expect even more sophisticated methods for creating bioengineered solutions that mimic or replace natural tissues.
The benefits are profound—enhanced quality of life, reduced dependency on donor organs, and potential cures for previously untreatable conditions. However, these innovations also come with challenges and ethical dilemmas that require careful navigation.
Understanding how artificial organs work paves the way for future developments in this field. With ongoing research aimed at overcoming current limitations, the future of tissue engineering holds exciting possibilities.
As we continue to explore this evolving landscape, it’s clear that the intersection of biology and technology will play a crucial role in shaping healthcare as we know it today and tomorrow.